In 2017, areas of northern New South Wales experienced significant flooding as a result of ex-Tropical Cyclone Debbie. Such events are likely to become more frequent and severe due to climate change. There is a current gap in the literature investigating the effects of indirect disruption caused by flooding (e.g. loss of access to health and social care for people who have not had their property inundated) on mental health. A survey was conducted of flood-affected communities across northern New South Wales six months after the event to investigate relationships between the flood and adverse mental health outcomes. Responses were used to investigate associations between indirect disruptions and psychological morbidity. Respondents who reported indirect disruption were significantly more likely to report experiences consistent with probable post-traumatic stress disorder than those who did not report any disruption. Those who reported a loss of health and social care or a disruption to their utilities were more likely to experience adverse mental health outcomes. This study showed that indirect disruption due to flooding is associated significantly with adverse mental health. Post-disaster recovery managers might consider allocating mental health support for people who have experienced indirect disruptions.
Introduction
Recent years have seen a growing literature on the mental health and wellbeing of individuals affected by flooding (Fernandez et al. 2015). Much of the focus has been on the relationship between direct disruption due to flooding and poor mental health (Alderman, Turner & Tong 2012; Zhong et al. 2018; Waite et al. 2017; Jermacane et al. 2018; Reacher et al. 2004; Paranjothy et al. 2011; Fontalba-Navas et al. 2017; Milojevic et al. 2011). Inundation of property, damage to possessions and forced evacuations due to flooding can all be classified as direct disruptions. A key finding regarding direct disruptions has been their significant association with post-traumatic stress disorder (PTSD) (Waite et al. 2017; Munro et al. 2017; Jermacane et al. 2018; Zhong et al. 2018; Alderman, Turner & Tong 2013; Paranjothy et al. 2011; Matthews et al. 2019)
Conversely, there is a dearth of published research investigating the associations between mental health morbidity and indirect disruptions such as losing access to health care, food or place of employment for people who have not had their property inundated with flood water. Two of the only studies of indirect disruptions following flooding events come from England. These studies identified adverse effects on mental health, especially PTSD (Paranjothy et al. 2011, Waite et al. 2017). To date, there has been no research on the mental health effects of indirect disruptions published in the Australian context.
Objectives
The objectives of this research:
- Examine the associations between an experience of indirect disruption and direct disruption with mental health outcomes after a flood.
- Examine which types of indirect disruption due to flooding are most strongly associated with adverse mental health outcomes.
Study design
From September to November 2017, six months after ex-Tropical Cyclone Debbie caused extensive flooding in northern New South Wales, a cross-sectional survey was implemented targeting people who had been living in six local government areas of Ballina Shire, Tweed Shire, Richmond Valley, Kyogle, Byron Shire and Lismore City at the time of the flood. These areas had an estimated population of 247,000 (Australian Bureau of Statistics 2017). Community members aged 16 years and older were recruited using a ‘snowball’ sampling method. This method incorporated social and organisational networks of local government authorities, business groups and community organisations and was supplemented by an extensive local advertising campaign using print, broadcast and social media. This included a leaflet drop in the two largest centres of population flooded; Lismore and Murwillumbah. All residents were encouraged to participate whether or not they felt the flood had affected them. The survey was available in online and paper formats. Potential respondents were advised that completion of the questionnaire would signify consent to participate in the study. A detailed description of the study design was published by Longman and colleagues (2019).
The study was approved by the University of Sydney Human Research Ethics Committee (reference-2017/589) and the Aboriginal Health and Medical Research Council Human Research Ethics Committee (reference-1294/17).
Measures of disruption
The survey contained questions relating to the degree of flooding, disruption, socio-demographic characteristics and the mental health and wellbeing of the respondents. Using the responses to the disruption questions, participants were categorised into three independent groups: directly disrupted, indirectly disrupted and non-disrupted (Waite et al. 2017).
Directly disrupted respondents: Those who reported flooding or damage to any area of their home or income-generating property (e.g. business or farm). These respondents had answered yes to at least one of the following questions:
- Were non-livable areas of your home damaged or flooded (e.g. garage, garden shed)?
- Was at least one livable room in your home damaged or flooded (e.g. bedroom, living room, kitchen, bathroom)?
- If you own a business, was it damaged or flooded (e.g. if you own a shop, farm, warehouse)?
Indirectly disrupted respondents: Those who were not flooded (i.e. answered ‘No’ to all the previous questions) but who answered yes to any of the following:
- Your access to health and social care was disrupted.
- You had difficulty getting the food supplies you needed.
- You were temporarily isolated as surrounding roads were cut.
- You were unable to travel to your place of education (e.g. school, university, TAFE).
- There were interruptions to your household utilities (e.g. electricity, gas, drainage, septic).
- Your Wi-Fi/internet stopped working.
- You were unable to travel to your place of employment.
Non-disrupted respondents: Those who reported none of the specified disruptions.
Measures to assess mental health
Previous studies of disasters including flooding have indicated that PTSD, depression, anxiety and increased suicide risk are common sequelae (Alderman, Turner & Tong 2013; Paranjothy et al. 2011; Waite et al. 2017; Zhong et al. 2018; Tang et al. 2018; Lowe et al. 2019). Therefore, in this study, mental health status was assessed using brief versions of validated screening tools of:
- the Patient Health Questionnaire (PHQ-2) for depression (Kroenke, Spitzer & Williams 2003)
- the Generalised Anxiety Disorder scale (GAD-2) (Kroenke et al. 2007)
- the Post Traumatic Stress Disorder Checklist (PCL-6) (Lang & Stein 2005, Fernandez et al. 2015).
The PHQ-2, GAD-2 and PCL-6 were selected to keep the outcomes of this study in-line with the only other study previously published investigating the comparison between disruption type due to flooding and adverse mental health outcomes (Waite et al. 2017).
Cut-points for probable diagnosis were ≥3 for the PHQ-2 and GAD-2 and ≥14 for the PCL-6 (Lang & Stein 2005; Kroenke, Spitzer & Williams 2003; Kroenke et al. 2007). To relate responses to the PCL-6 to the flood, the checklist was introduced as a list of complaints that people express after extreme rain and flooding. Additional mental health measures included an indicator of suicidal ideation from the Screening Tool for Assessing Risk of Suicide (Hawgood & DeLeo 2017) and an indicator of continuing distress six months after the flood (Clemens et al. 2013).
Socio-demographic measures
Socio-demographic data included age, gender, Indigenous status, relationship status, education level, employment status and government income support status. Only respondents with complete socio-demographic data were included in the analysis.
Analysis by disruption category
The analysis was conducted in two stages. First, binary logistic regression models were constructed to calculate the odds of experiencing each of the five types of mental health outcomes: continuing distress, suicidal ideation, probable depression, anxiety and PTSD. Respondents who did not complete a particular health outcome measure were excluded from analysis for that outcome. The dependent variables were the category of disruption, with non-disruption as the reference group. The models were adjusted for all measured socio-demographic characteristics. Sensitivity analyses were conducted to assess the level of bias introduced by including these characteristics.
Analysis by type of indirect disruption
In the second stage of the analysis, five multivariate logistic regression models were constructed that considered the association between each type of indirect disruption with each of the five mental health conditions as an outcome.
It was reasoned that a substantial portion of participants who experienced an indirect disruption was likely to also have experienced direct disruption. Therefore, only analysing the participants who experienced an indirect disruption without direct disruption would have resulted in a markedly reduced sample from which conclusions could be drawn and could introduce risk of bias in the results. For this reason, every participant who reported an indirect disruption was included and participants were not grouped by disruption category. To account for potential confounding caused by experiencing both direct and indirect disruption, the regression models included a binary variable that indicated any experience of direct disruption by the participants. Again, each model was adjusted for socio-demographic characteristics.
The interest was in identifying significant associations and important confounders. As such, purposeful selection was employed to construct the multivariate logistic regression models. Consistent with the purposeful selection method, other indirect disruptors were retained in the model if they demonstrated a p-value of less than 0.15 or if they demonstrated significant confounding effects (Δβ > 20%) (Bursac et al. 2008). As there were multiple analyses investigating the mental health outcomes in both sets of analyses, the α for significance testing was set conservatively at 0.01. Every regression model produced in this study was tested for effect modifications (α=0.01). Stata 15 ( Stata/SE 15.1 for Windows) was used for all statistical analyses.
Results
Respondent characteristics
In total, 2530 people responded to the survey and 350 (14 per cent) of the responses were missing socio-demographic data. Therefore, the analysis conducted using socio-demographic data was performed using a sample of 2180 participants. Negligible dissimilarities in parameter estimates and patterns of results were found between the full dataset and the dataset absent of missing socio-demographic records.
Mental health outcomes by disruption category
Of these 2180 respondents, 105 could not be classified into disruption categories due to incomplete survey responses, 242 respondents were classified as non-disrupted, 605 were classified as indirectly disrupted and 1228 were classified as directly disrupted. In total, 2075 respondents were included in this part of the analysis. Most of the respondents were over 45 years of age, were female, in a relationship and employed (Table 1, Appendix 1).
Among those who were classified as directly disrupted, between 10 per cent and 33 per cent demonstrated evidence of mental health distress in the outcomes measured. By comparison, among those who were classified as non-disrupted, between 2 and 8 per cent reported mental health distress (Table 2). Accordingly, the differences in proportions demonstrating evidence of mental health distress between the two groups ranged from 7 per cent (suicidal ideation) to 25 per cent (still distressed).
The differences in proportions demonstrating evidence of mental health distress between those classified as indirectly disrupted and non-disrupted was less stark, ranging from 1 per cent (suicidal ideation) to 7 per cent (probable anxiety).
When factoring in potential confounders in the logistic regression model, the greatest effect on the odds of probable PTSD was found in respondents who experienced direct disruption (OR: 14.4; 95 per cent, CI 5.9–35.3) (Table 3). After adjusting for socio-demographic factors, probable PTSD remained strongly associated with direct disruption (OR:13.5; 95 per cent, CI: 5.5–33.4). Indeed, the odds of experiencing every mental health outcome remained significantly elevated in response to direct disruption after adjusting for socio-demographic factors (Table 3).
Respondents categorised as indirectly disrupted were significantly more likely to experience probable PTSD, probable anxiety or still feel distressed than those who were categorised as non-disrupted. After adjusting for socio-demographic factors, only the odds of probable PTSD remained significantly elevated (OR: 3.52, 95 per cent, CI: 1.36–9.15) (Table 3).
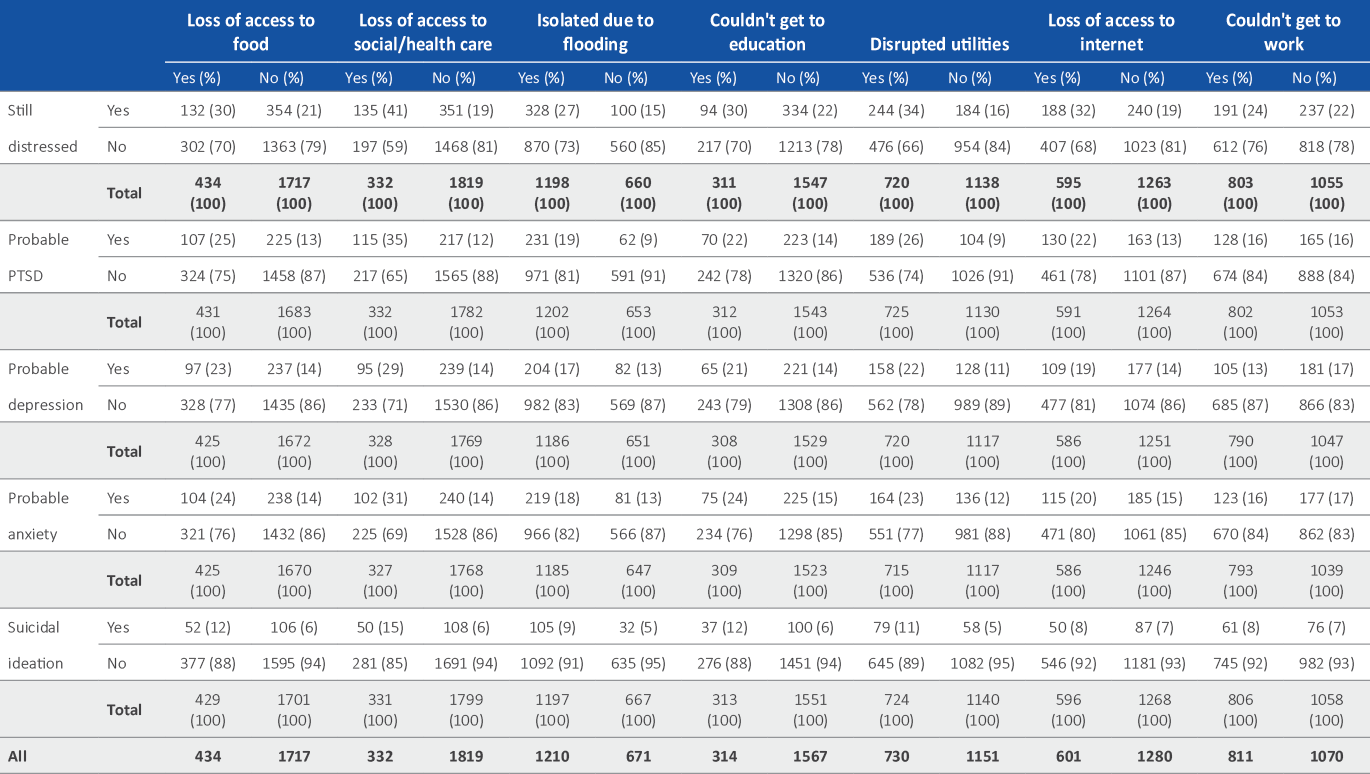
Mental health outcome by indirect disruption type
The relationships between each mental health outcome and each of the indirect disruption types were also examined using multivariate logistic regressions (n=2180).The other indirect disruptions were added to the models according to the purposeful selection method and were also adjusted for any experience of direct disruption and socio-demographic factors.
Loss of access to social or health care was shown to significantly increase the odds of every outcome except probable depression. No individual disruption type significantly influenced the odds of having probable depression (Table 5). On the outcome of probable anxiety, employment status significantly modified the size of the effect of a loss of access to health and social care. Among those participants who experienced a loss of access to health and social care, unemployed participants demonstrated greater odds of probable anxiety than those who were employed (OR: 2.67; 95 per cent, CI: 1.64, 4.35 vs OR: 1.05; 95 per cent, CI: 0.67, 1.64, respectively). A loss of utilities was strongly associated with every mental health outcome although this effect was only statistically significant for probable PTSD (OR: 1.9, 95 per cent, CI: 1.41–2.56) (Table 5).
Table 1: Socio-demographic characteristics of respondents by disruption category.
| Demographic | Disruption Category | ||||
| No disruption | Indirectly | Directly | Total | ||
| Age (years) | 16 to 25 | 8 (3%) | 37 (6%) | 65 (5%) | 110 (5%) |
| 24 to 45 | 51 (21%) | 173 (29%) | 290 (24%) | 514 (25%) | |
| 45 to 65 | 115 (48%) | 296 (49%) | 667 (54%) | 1078 (52%) | |
| 65 and older | 68 (28%) | 99 (16%) | 206 (17%) | 373 (18%) | |
| Total | 242 (100%) | 605 (100%) | 1228 (100%) | 2075 (100%) | |
| Gender | Female | 163 (67%) | 430 (71%) | 834 (68%) | 1427 (69%) |
| Male | 79 (33%) | 175 (29%) | 394 (32%) | 648 (31%) | |
| Total | 242 (100%) | 605 (100%) | 1228 (100%) | 2075 (100%) | |
| Aboriginal or Torres Strait Islander peoples | Yes | 9 (4%) | 14 (2%) | 53 (4%) | 76 (4%) |
| No | 233 (96%) | 591 (98%) | 1175 (96%) | 1999 (96%) | |
| Total | 242 (100%) | 605 (100%) | 1228 (100%) | 2075 (100%) | |
| Relationship status | In a relationship | 162 (67%) | 414 (68%) | 820 (67%) | 1396 (67%) |
| Single | 80 (33%) | 191 (32%) | 408 (33%) | 679 (33%) | |
| Total | 242 (100%) | 605 (100%) | 1228 (100%) | 2075 (100%) | |
| Education attained | University | 119 (49%) | 304 (50%) | 483 (39%) | 906 (44%) |
| Other | 123 (51%) | 301 (50%) | 745 (61%) | 1169 (56%) | |
| Total | 242 (100%) | 605 (100%) | 1228 (100%) | 2075 (100%) | |
| Employment status | Employed | 143 (59%) | 450 (74%) | 835 (68%) | 1428 (69%) |
| Other | 99 (41%) | 155 (26%) | 393 (32%) | 648 (31%) | |
| Total | 242 (100%) | 605 (100%) | 1228 (100%) | 2075 (100%) | |
| Income support | None | 165 (68%) | 451 (75%) | 800 (65%) | 1416 (68%) |
| Support | 77 (32%) | 154 (25%) | 428 (35%) | 659 (32%) | |
| Total | 242 (100%) | 605 (100%) | 1228 (100%) | 2075 (100%) | |
Table 2: Respondent mental health outcome by disruption category.
| Outcome | Overall cohort | Disruption Category | ||
| Non-disrupted | Indirectly | Directly | ||
| Still distressed | 478/2050 (23%) | 20/242 (8%) | 58/597 (10%) | 400/1211 (33%) |
| Probable PTSD | 327/2044 (16%) | 5/232 (2%) | 40/599 (7%) | 282/1213 (23%) |
| Depression | 326/2026 (16%) | 13/235 (6%) | 57/590 (10%) | 256/1201 (21%) |
| Probable anxiety | 335/2021 (17%) | 9/232 (4%) | 62/590 (11%) | 264/1199 (22%) |
| Suicidal ideation | 156/2056 (8%) | 8/240 (3%) | 23/601 (4%) | 125/1215 (10%) |
| Total* | 2075 | 242 | 605 | 1228 |
* Totals differ from the overall sample size due to missing responses for outcome and exposure reporting.
Table 3: Crude and adjusted odds ratios (OR) for mental health problems by disruption category.
| Outcome | Disruption group | n | Crude OR | Crude P-value | n | Adjusted OR# | Adjusted P-value |
| Still distressed | Non-disrupted | 260 | 1Ɨ | - | 246 | 1Ɨ | - |
| Indirectly | 654 | 1.21 (0.72–2.05) | <0.001 | 597 | 0.95 (0.47–1.89) | 0.878 | |
| Directly | 1374 | 5.77 (3.6–9.23) | <0.001 | 1211 | 3.31 (1.79–6.12) | <0.001 | |
| Probable PTSD | Non-disrupted | 246 | 1Ɨ | - | 232 | 1Ɨ | - |
| Indirectly | 646 | 3.52 (1.38–8.99) | 0.008 | 599 | 3.52 (1.36–9.15) | 0.01 | |
| Directly | 1341 | 14.43 (5.9–35.31) | <0.001 | 1213 | 13.48 (5.45–33.35) | <0.001 | |
| Probable depression | Non-disrupted | 249 | 1Ɨ | - | 235 | 1Ɨ | - |
| Indirectly | 639 | 1.88 (1.01–3.49) | 0.045 | 590 | 1.9 (1–3.62) | 0.05 | |
| Directly | 1331 | 4.99 (2.81–8.86) | <0.001 | 1201 | 4.26 (2.35–7.73) | <0.001 | |
| Probable anxiety | Non-disrupted | 247 | 1Ɨ | - | 232 | 1Ɨ | - |
| Indirectly | 639 | 2.56 (1.33–4.92) | 0.005 | 590 | 1.55 (0.7–3.44) | 0.279 | |
| Directly | 1325 | 6.09 (3.28–11.3) | <0.001 | 1199 | 3.64 (1.74–7.62) | 0.001 | |
| Suicide ideation | Non-disrupted | 256 | 1Ɨ | - | 240 | 1Ɨ | - |
| Indirectly | 648 | 1.24 (0.55–2.8) | 0.597 | 601 | 1.02 (0.44–2.35) | 0.961 | |
| Directly | 1340 | 3.47 (1.68–7.18) | 0.001 | 1215 | 2.86 (1.36–5.99) | 0.005 |
# Adjusted for age, gender, Indigenous status, receiving income support, education and relationship status.
Ɨ Reference group.
Discussion
The strong link between disruption after a flood event and PTSD has been clearly elucidated in recent literature (Fontalba-Navas et al. 2017, Zhong et al. 2018, Dai et al. 2017, Waite et al. 2017, Paranjothy et al. 2011, Fernandez et al. 2015, Matthews et al. 2019). Consistent with Waite and co-authors (2017), these results showed a significant association between direct disruption and probable PTSD. By comparison, significant association has also been demonstrated between indirect disruption and probable PTSD, although the strength of association is comparatively weaker. This apparent dose-response relationship offers evidence for the causative relationship between the level of disruption due to flooding and the outcome of probable PTSD.
Direct disruption also demonstrated significant associations with the other four mental health outcomes when compared with non-disruption, namely: still distressed, probable depression, probable anxiety and suicidal ideation. By contrast, no significant associations were found between indirect disruption and these four mental health outcomes.
This is one of the few studies that has sought to investigate the associations between mental health and indirect disruption due to a flooding event. Consistent with previous research, indirect disruption was found to be significantly associated with an increased risk of probable PTSD in comparison with individuals classified as non-disrupted (Waite et al. 2017, Paranjothy et al. 2011).
To date, there has been little discussion in the literature about mechanisms that might account for this increased risk of probable PTSD in cases where there has been disruption experienced, albeit with no direct damage to people’s homes or businesses. Some indications of possible mechanisms might be derived from research on the impact of near-miss experiences and PTSD diagnostic criteria.
Recent literature on ‘near-miss experiences’ following traumatic events suggests that people who have had near-miss events tend to experience more intrusive thoughts about what might have been and are more likely to think about the actual misfortune of others, which may reinforce intrusions and raise the likelihood of post-traumatic stress symptoms (Poulin & Silver 2019). It might be inferred that those who experienced indirect disruption had a ‘near-miss experience’ and may have been more sensitive to what might have been and therefore more prone to post-traumatic stress than those who were classified as non-disrupted.
Except for probable depression, these results demonstrate a strong association between losing access to health and social care and every mental health outcome investigated. A similar association was reported by Waite and colleagues (2017), although their results were not mutually adjusted for other disruption types. Interruption to household utilities was also shown to significantly increase the odds of having probable PTSD, consistent with similar findings reported related to the loss of electricity after a flooding event in Hat Yai, Thailand (Assanangkornchai, Tangboonngam & Edwards 2004).
People who lost access to health and social care as well as being unemployed, were more likely to have an outcome of probable anxiety than those who were employed. It may be that people experiencing unemployment are more likely to need access to health and social care than people who are employed. It may also be that unemployment as well as a loss of this access may have a cumulative effect on anxiety.
There were increased odds of reporting probable PTSD for participants who were classified as indirectly disrupted and for those who specifically reported either a disruption of access to social and health care or a disruption to utilities. Therefore, it is possible that the association between an experience of indirect disruption and the outcome of probable PTSD is largely explained by losing access to social or health care and/or a disruption to utilities.
Given the predicted intensification of the effects of climate change (Climate Council 2017), there is likely to be an increasing number of people who are disrupted by flooding events. This study offers evidence that after a flooding event those in need of mental health support will include people who have been directly disrupted and also those who have lost access to social and health care as well as those who have experienced a disruption to utilities provision.
Treatment of mental health problems, including PTSD, following disasters requires specific training for those working in the mental health field (Foa, Gillihan & Bryant 2013). Furthermore, it is recognised that different approaches delivered by professionals may be needed at different stages post disaster (Forbes, O'Donnell & Bryant 2017). Given the findings of this study, it may be prudent to provide the health care workforce with access to appropriate-level training (e.g. mental health first-aid for the general health and community sector, PTSD training for specialists) in preparation for future acute events. Part of this training could involve how to identify people most in need of mental health care, including those who have been indirectly disrupted. Also, given that those who require mental health support after a flood event may need assistance more than six months after a flooding event (Zhong et al. 2018), planning is needed to provide support in the longer, not just immediate, term.
Table 4: Multivariate logistic regression models for mental health outcomes and individual indirect disruption types.
| Mental health outcome | Contributing variable | Adjusted odds ratio (95% CI) | P-value |
| Still distressed | Loss of access to social or health care | 8 (3%) | |
| No loss of access | 1 | - | |
| Loss of access** | 1.86 (1.38–2.49) | <0.001 | |
| Loss of utilities | |||
| No loss of access | 1 | - | |
| Loss of access | 1.34 ( 1.02–1.75) | 0.034 | |
| Loss of access to internet | |||
| No loss of internet | 1 | - | |
| Loss of internet | 1.4 (1.08–1.82) | 0.012 | |
| Probable PTSD | Loss of access to social or health care | ||
| No loss of access | 1 | - | |
| Loss of access** | 1.93 (1.38–2.7) | <0.001 | |
| Loss of utilities | |||
| No loss of utilities | 1 | - | |
| Loss of utilities** | 1.9 (1.41–2.56) | <0.001 | |
| Difficulty accessing food | |||
| No difficulty | 1 | - | |
| Difficulty | 1.31 (0.94–1.83) | 0.105 | |
| Probable depression | Loss of access to social or health care | ||
| No loss of access | 1 | - | |
| Loss of access | 1.51 (1.44–2.82) | 0.016 | |
| Loss of utilities | |||
| No loss of utilities | 1 | - | |
| Loss of utilities | 1.38 (1.02–1.85) | 0.035 | |
| Probable anxiety^ | Loss of access to social or health care | ||
| Not employed/No loss of access | 1 | - | |
| Not employed/Loss of access** | 2.67 (1.64–4.35) | <0.001 | |
| Employed/No loss of access | 1 | - | |
| Employed/Loss of access | 1.05 (0.67–1.64) | 0.838 | |
| Loss of utilities | |||
| No loss of access | 1 | - | |
| Loss of access | 1.31 (0.98–1.74) | 0.07 | |
| Suicide ideation | Loss of access to social or health care | ||
| No loss of access | 1 | - | |
| Loss of access* | 1.74 (1.14–2.66) | 0.01 | |
| Loss of utilities | |||
| No loss of access | 1 | - | |
| Loss of access | 1.43 (0.96–2.13) | 0.079 |
Each model is adjusted for age, gender, Indigenous status, receiving income support, education, relationship status and an experience of direct disruption; remaining covariates retained and presented as per the purposeful selection method.
^Denotes significant effect modification identified (α=0.01)
* Denotes p-value ≤ 0.01.
** Denotes p-value ≤ 0.001.
Limitations
The self-selection recruitment method means the respondent population is not representative of the population of the flood-affected communities of northern New South Wales. In this study, men, those with less education and those under 25 years of age were under-represented, which is consistent with previous post-disaster postal survey respondent characteristics (Grievink et al. 2006). However, this study did not aim to establish prevalence of mental health outcomes after flooding, but rather to examine the relationships between levels and types of disruption and mental health status. Further, to ascertain the relationships of interest, a study’s population does not necessarily have to be representative of the general population from which it was derived (Willett et al. 2007, Banks et al. 2008).
Conclusions
The responses to the community survey conducted in northern New South Wales have contributed to knowledge around mental health effects after a significant flooding event (Matthews et al. 2019). The findings are consistent with, and extend, what has been presented in recent literature. It is proposed that people experiencing disruptions to social and health care services or utilities after a flood might be targeted for mental health support.
Further research in this area might investigate causal mechanisms behind indirect disruptions and their associated mental health outcomes. Also, planned follow-up surveys involving respondents who have indicated an interest in future participation may shed light on the longer-term mental health consequences of flooding events.
Appendix i. Number and proportions of respondents reporting mental health outcomes for each indirect disruption type.