Landmark Australian research into the mental health, wellbeing and suicide risk of 21,014 police and emergency services personnel has established national baseline measures and given agencies and stakeholders clear evidence to underpin and drive action.
The Answering the call national survey – Phase 2 of Beyond Blue’s National Mental Health and Wellbeing Study of Police and Emergency Services was commissioned and funded by Beyond Blue with a funding contribution from the Bushfire and Natural Hazards Cooperative Research Centre. Professor David Lawrence at the University of Western Australia led the survey in partnership with Roy Morgan Research. The research was released on 29 November 2018.
Despite several smaller-scale research studies and extensive, anecdotal evidence that police and emergency services personnel are at greater risk of experiencing a mental health condition, until now, no comprehensive, national data existed. This has created challenges in understanding the true extent of psychological distress, mental ill health and suicide risk in the sector.
This research provides a detailed and accurate picture of these issues across Australia. We now have national baseline measures of wellbeing, mental health conditions and suicide risk among police and emergency services personnel. These can be used to drive action, design strategies and support services that respond to the data, including issues that police and emergency services personnel say are important as well as measure progress.
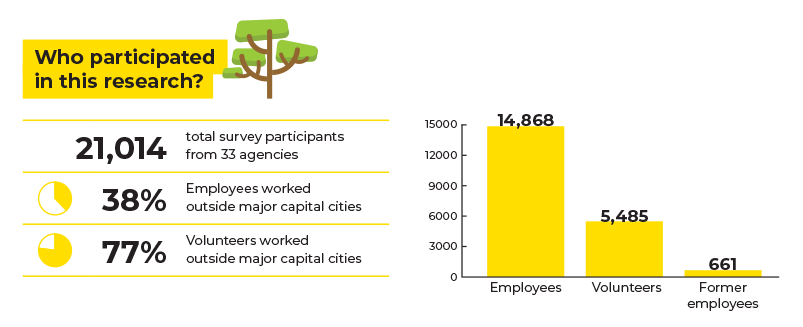
The survey was conducted from October 2017 to March 2018 and involved current employees (operational and non-operational), current volunteers and former and retired employees working in ambulance, fire and rescue, police, and state emergency service agencies in each Australian state and territory.
Of the 36 agencies in the sector, 33 participated in the survey. In total, 21,014 respondents (14,868 employees and 5485 volunteers) participated in the voluntary survey meaning representative samples were achieved for these groups. In addition, a sample of 661 former employees was recruited through associations of former employees and related groups.
The survey measured mental health and wellbeing outcomes across nine themes.
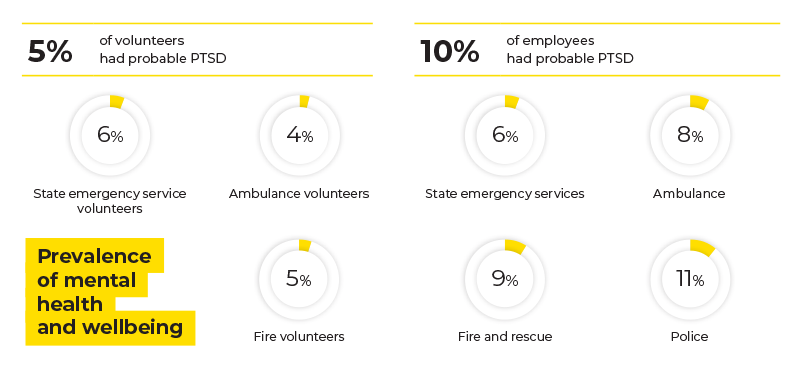
Prevalence of mental health and wellbeing
The survey found that ten per cent of employees had probable post-traumatic stress disorder (PTSD). Rates of PTSD ranged from 6 per cent in the state emergency services sector, 8 per cent in ambulance, 9 per cent in fire and rescue to 11 per cent in police. In comparison, the prevalence of PTSD has been estimated at 4 per cent in adults in Australia and 8 per cent in the Australian Defence Force.
Twenty-one per cent of employees had high psychological distress and 9 per cent had very high psychological distress; much higher than the 8 per cent and 4 per cent respectively for all Australian adults.
Volunteers showed lower levels of psychological distress and probable PTSD and higher levels of positive wellbeing, with 4 per cent of ambulance volunteers, 5 per cent of fire and rescue volunteers and 6 per cent of state emergency service volunteers having probable PTSD.
Suicidal thoughts and behaviours
Suicidal thoughts and planning were more than twice as common in employees and volunteers compared to the Australian population, however rates of suicide attempts were comparable with the general population. Employees with higher levels of social support and resilience reported lower levels of suicidal thoughts and behaviours, even if they had experienced traumatic events that deeply affected them in their work or were likely to have PTSD.
Individual risk and protective factors
Employees and volunteers who had started their career in the previous two years had high levels of mental wellbeing and very low levels of psychological distress, probable PTSD and suicidal thoughts. Higher rates of psychological distress and probable PTSD were associated with greater length of service (ten years or more), low levels of social support and more exposure to traumatic events that deeply affected individuals.
More than 80 per cent of employees and 90 per cent of volunteers reported providing high levels of social support to others, as well as receiving similar support.
Different groups of people involved in the survey had their prevalence of mental health and wellbeing measured across nine different themes. Image: Bushfire and Natural Hazards CRC
Substance use
Many police and emergency services employees reported high rates of alcohol consumption, which may indicate its use for coping with stress or poor mental health.
Almost 50 per cent of employee alcohol consumption exceeded National Health and Medical Research Council guidelines. Sixteen per cent of employees drank five or more drinks in a single session at least weekly, and 17 per cent drank ten or more drinks in a single session in the previous month.
Rates of illicit drug use were comparatively low. About 5 per cent of employees reported having used illicit drugs within the past year, although 13 per cent of employees with probable PTSD reported doing so. This compares to 16 per cent of Australians aged 14 and older who reported using illicit drugs over a 12-month period.1
Risk and protective factors associated with the working environment
The workplace environment, particularly poor team culture and workplace stress factors, such as inadequate resources and unpaid overtime, had significant impacts on the mental health of employees. In fact, the study found that poor workplace practices and culture were just as debilitating as exposure to trauma.
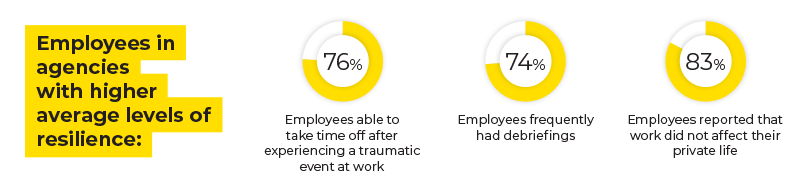
Where higher levels of resilience were found, this was accompanied by more employees reporting that they were able to take time off after experiencing a traumatic event at work, they had briefings more frequently andwork did not drain so much energy as to affect their private life.
Stigma
The revealed clear disparities in the way people feel about their colleagues and how they see themselves Employees and volunteers tended to believe that others in the workplace held negative beliefs towards those with a mental health condition or a low commitment to support those with mental health conditions. Employees held notable levels of stigma surrounding their own mental health. Thirty-three per cent of respondents felt shame about their mental health condition and 61 per cent said they would avoid telling people about their mental health condition. Despite these figures, most employees and volunteers reported they would support any colleague who experienced a mental health condition.
The research will guide agencies to develop, refine and implement better and longer-term mental health and wellbeing programs. Image: Bushfire and Natural Hazards CRC
Seeking support
Comparatively, more people in the police and emergency services sector seek support when they need it for a mental health condition than in the Australian population overall. Barriers to seeking support commonly cited, for employees and volunteers alike, included wanting to deal with it themselves, concerns about being treated differently or being perceived as weak.
Nearly half of employees believed they had received sufficient support for their needs, which is comparable with the general population.
Workers’ compensation
Most respondents making workers’ compensation claims found the process to be unsupportive, stressful and reported that it had a negative impact on their recovery. Among employees with probable PTSD who made a claim, 75 per cent felt it had negative impacts on their recovery, with only 8 per cent reporting positive impacts on their recovery. More than half (52 per cent) felt they were not supported at all during the claims experience, and 63 per cent reported that they found the claims experience to be very or extremely stressful.
Former employees
Twenty-eight per cent of former employees had seriously thought about taking their own life. Of those, 66 per cent felt this way while still working in the police and emergency services sector and 62 per cent felt this way after leaving the sector.
Former employees had lower resilience and were much less likely to receive high levels of social support compared with current employees, particularly those former employees currently having probable PTSD or high rates of psychological distress.
How the research is being used
Beyond Blue has analysed the findings and made independent recommendations. Phase 3 of the study is to translate the findings into more action.
The research shows there are many common themes at a national level. We believe a nationally coordinated approach—led by the Commonwealth—to respond to the findings will lead to better outcomes for individuals and families more quickly and with less duplication. We have recommended a national centre of excellence for police and emergency services mental health to be a hub of proven and emerging best practice and outcomes, that reforms to workers’ compensation are driven by a review of current practices and best-case solutions and that a scheme to support post-service employees and retirees is imperative.
Beyond Blue has also recommended agencies review their existing health and wellbeing strategies and plans against the evidence produced by the research. Strategies should be fully integrated into core business and developed collaboratively with peak bodies, unions, employees, volunteers and their families.
While the research findings are hard to read, we now have a comprehensive national picture and data set and a clear path to respond to the mental health needs of those who put their lives on the line for others.
Footnotes
- 2016 National Drug Strategy Household Survey, Australian Institute of Health and Welfare.


