AIIMS Health check
Stephen Luke
Stephen Luke continues his Emergency Services Foundation scholarship project with discussion to better integrate Health and mainstream incident management systems
Article
Australia’s medical services are a complex functional grouping of planners, practitioners, health professionals, service organisations and government agencies (generically referred to in this paper as ‘Health’) that share many similarities with mainstream emergency management. Despite this, Health remains at the periphery of incident management frameworks, including the Australasian Inter-service Incident Management System (AIIMS). Many opportunities exist to increase the inclusion of Health in mainstream incident management. This paper considers a range of aspects including mass gatherings and recommendations from reviews of previous events like the Boston Marathon bombing.
Introduction
Primacy of life is the fundamental motivator and a universally accepted core value of emergency management agencies and personnel. The number of injuries sustained and lives lost are a significant determinant of a disaster’s impact. Despite this, Health, as a complex functional agency, is strangely absent from many facets of mainstream incident management practice. This is illustrated by the lack of prominence Health has in the AIIMS framework.
Disasters of national significance in Australasia have increased fivefold over the past 25 years (Bradt et al. 2015). Significant emergency management reform is underway as a result of the findings and recommendations from reviews into high-profile disasters, with many themes common to Royal Commission reports dating back over 100 years. Despite being integral to emergency management planning and response, Health continues to languish as a support unit within the logistics arm of the AIIMS Functional Management model (see Figure 1).
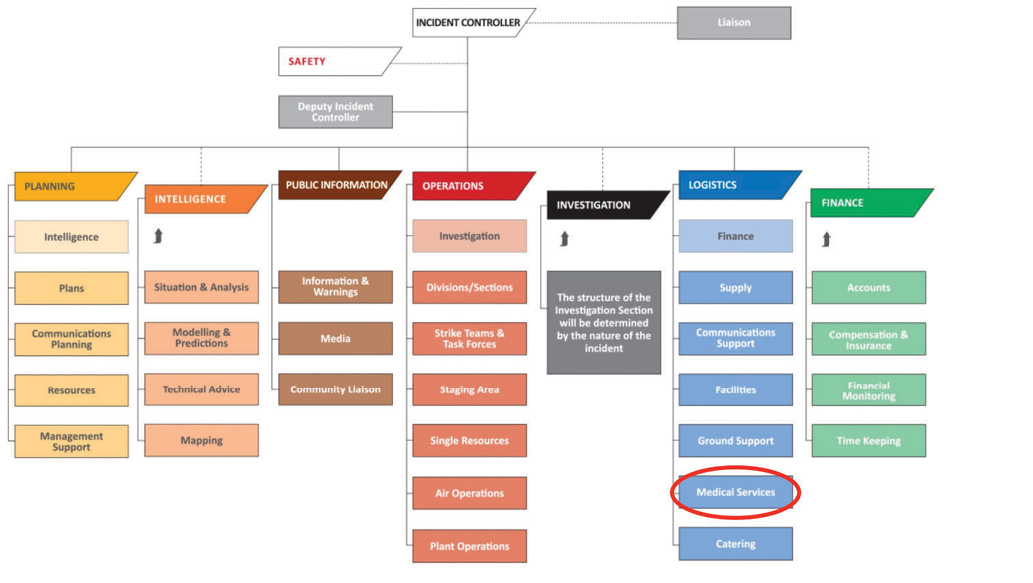
Figure 1: Medical Services (Health) location within the AIIMS4 Incident Control Structure.Source: Australasian Inter-Service Incident Management System (AFAC 2013).
Health is not an agency in the traditional emergency management sense. There is no single uniform or identity, yet in many ways Health typifies the challenges of multi-agency command. Health culture is confronting to outsiders and variants of different languages are spoken. Health is a complex and, at times, loosely bound network of organisations. Health includes a wide range of skilled practitioners from government, commercial and non-government organisations, spanning the hospital, pre-hospital, community, academic and bureaucratic domains.
Those working within Health manage many of the challenges in emergency management on a daily basis. These include:
- demand management
- balancing core service delivery needs with surge requirements and resource limitations
- maintaining standards
- minimising expense
- providing public emergency information and media management
- staff safety, rostering and fatigue management.
In Health, these manifest as an apolitical necessity to balance limited resources when managing ambulance services demand and emergency department and hospital capacity, balancing elective surgery with emergency hospital admissions, and coordinating in-patient and community rehabilitation, aged care services and mental health services. Health networks and systems are, and must be, inherently scalable and responsive to periods of increased demand, due to either daily workload changes or an emergency. This is a fundamental reality of modern healthcare delivery and the meeting of community expectations.
Despite numerous similarities and inherent structural synergy, the involvement of Health in mainstream emergency planning and incident response is often peripheral. This reflects Health agencies as playing a support role in an integrated incident response, for example providing the face of public health broadcasts, providing emergency care to the sick and injured, or providing first aid at community relief centres and fire staging grounds. Throughout this, there remains a strong parallel focus on the need for hospitals, health and ambulance services to continue ‘normal business’ operations. It is important to realise and be constantly aware that this might involve ambulance and mobile community health services, for example, responding into and providing ‘normal business’ services in disaster-affected areas, separate from resources tasked to the incident and potentially unknown to the controlling Incident Management Team.
Hospital Incident Management Teams
Hospital Incident Management Teams are often established to manage a Hospital and Health Service’s response to internal (Code Yellow) and external (Code Brown) emergencies. This is often done with limited direct interaction with non-health stakeholders. Furthermore, emergency incidents may appear minor to attending emergency services personnel but may have a significant impact on local health services. For example the need to evacuate a small rural health facility due to flood or fire (as occurred in the Charlton and Numurkah health facilities during the 2011 Victorian floods) or the loss of road access for ambulances due to road or bridge damage (e.g. loss of the Angellala Creek Bridge in south-west Queensland).
Hospitals are designed to be resilient and self-sufficient but remain susceptible to natural disasters and critical infrastructure failure. Examples include loss of power or telephone services, elevated demand on ambulance workload and patient acuity during heat wave, and the full evacuation of over 300 patients from the Cairns Base and Private hospitals, 1700 km to Brisbane in the lead up to Cyclone Yasi (Little et al. 2012, PricewaterhouseCoopers (PWC) 2011).
Isolated health emergencies occur less frequently. Infectious diseases outbreaks such as Pandemic Influenza and Ebola Viral Disease provide good clinical case studies and demonstrate how quickly critical infrastructure and other services can be directly affected. There is growing recognition of the health, social and economic importance of ‘Heat Health’. It is sobering to note that twice the number of people died in Victoria during the heat wave preceding the Black Saturday bushfires in February 2009 than the 173 lives lost during the fire event.
Vulnerable groups in communities
Heatwave is a long-standing and under-recognised global problem. Heatwave claimed 1500 lives in New York in 1896 and over 50,000 lives were lost in Europe in 2003 with 15,000 in France alone (Kohn 2010, PWC 2011). The vulnerability of individuals and communities to heat wave (and consequently temperature thresholds) vary widely and it is important that planning identify people and groups who are at highest risk of heat-related illness (Victorian Government 2014).
The complexity of Health and its interaction with emergency management is illustrated by work considering vulnerable people. Defining vulnerability is difficult and is contextually dependent on health and social determinants. For example, a person’s vulnerability may vary based on their exposure to temperature extremes, geographic or social isolation, transport limitations, or their dependence on power for life-support medical equipment. Even after the identification of vulnerabilities, the challenge continues for health providers, state-based health services, and local governments to maintain current lists and ‘lists of lists’, independent of Centrelink, Medicare and other government databases (Garlick 2015). These challenges continue throughout incident response and recovery phases.
Public health environments
Public health may quickly become a priority as a direct consequence of natural disasters. The health implications of air pollution during the Hazelwood coal mine fire in Gippsland in 2014 remain an active area of interest in a Victorian Government-commissioned inquiry. Food security and health services require reliable energy supplies and intact delivery mechanisms to support communities. Water and vector-borne diseases are a major health concern after destructive flood and storm events, especially where drinking water supplies and sewage treatment facilities are compromised. Emergency responses by Australian Medical Assistance Teams to assist islanders in the Pacific over the last decade (e.g. Banda Aceh, Haiti, Vanuatu, Tahiti, Fiji) have provided urgent primary care and public health interventions to treat and prevent disease, particularly in tropical and low socio-economic communities (NCCTRC 2015).
The health response ‘tail’
The health implications of a relatively short duration incident response may be protracted and consume significant resources long after emergency services responders clear the scene, as demonstrated by the Ravenshoe Café explosion in 2015 (see Dean 2015). The fire was extinguished quickly and the challenge became the treatment and medical evacuation of 21 injured patients to nearby hospitals, with 11 of these requiring aero-medical retrieval over 1500 km from north Queensland to the specialist burns unit in Brisbane (Queensland Government 2016). Burns patients require specialist and ongoing intensive treatment and additional capacity is readily available through the national AUSBURNPLAN and its parent document, AUSTRAUMAPLAN. These plans facilitate the distribution of patients throughout the Australian hospital system and have evolved in response to lessons learned from local and international mass casualty incidents, including the Bali, Madrid and London bombings (Australian Government 2011).
Existing Health emergency management
While highlighting the need for improved integration between mainstream and Health incident management, it is important to acknowledge the well-established frameworks, resources and training already in place to varying degrees around Australia. These are:
- Major Incident Medical Management and Support training courses
- development of national, state and territory health emergency plans, including AUSBURNPLAN and AUSTRAUMAPLAN
- the growth of the ambulance service as a profession and pre-hospital lead health agency
- establishment of a pre-hospital ‘Health Commander’ role in the Victorian Health Emergency Response Plan
- implementation of ambulance and hospital demand management practices
- development of Hospital External Emergency (Code Brown) plans in accordance with Australian Standards
- emergency management training for hospital management
- joint hospital, ambulance and emergency services Emergotrain SystemTM and field exercises
- continuing work on the definition and management of ‘vulnerable people’ across a range of different emergencies.
Health emergency management systems and resources have improved greatly with the development of dedicated Health Disaster Management Teams, triggered initially by responses to disasters like Cyclone Tracy (1974), the Granville train disaster (1977), and Ash Wednesday (1983) (Bradt et al. 2015). More recently, the Health responses to the Victorian Black Saturday bushfires in 2009 and the Brisbane floods in 2011 demonstrate the need for prolonged Health involvement in relief and recovery operations. This is particularly in areas of the management of chronic medical conditions, loss of medications, and monitoring the mental health of affected and displaced persons (Luke 2013). With climate change expected to increase the frequency and impact of heat wave and other natural disasters, improved and integrated planning is required to increase response capacity and build resilience.
Health resilience is promoted throughout the United Nations-endorsed Sendai Framework for Disaster Risk Reduction 2015-2030, successor to the The Hyogo Framework for Action 2005-2015. These frameworks promote disaster risk reduction as a proven, cost-efficient means of reducing loss of life and social, economic and environmental assets (UNISDR 2005, 2015). This global framework is acutely relevant in Australasia with a recent epidemiological evaluation showing a fivefold increase in disasters of national significance over the last 25 years (Bradt et al. 2015).

The Boston marathon bombing demonstrates the importance of active Health involvement in all phases of mass gathering and emergency management. Image: Aaron Tang, Wikimedia Commons.
Response scalability and mass gatherings
Successful emergency management systems rely heavily on professional networks, efficient communication, and response capacity with inherent scalability. Small incidents can escalate quickly and with little notice, reinforcing the importance of the ‘train as you fight, fight as you train’ principle. The Boston Marathon bombing in 2013 is an excellent example of how quickly a planned event can escalate to an emergency and mass casualty incident. In their review, Why Was Boston Strong? Lessons from the Boston Marathon Bombing, Leonard and colleagues (2014) highlight the importance of established plans and relationships in the success of the response. The presence of the on-site medical team at the finish line and the planned activation of the city coordination centre to oversee the distribution of patients across its hospitals were critical to the success of the emergency health response and the number of lives saved.
Leonard and colleagues (2014) identified the value of mass gatherings for emergency management training:
“Fixed” or planned events can be effective platforms for practicing incident management skills even when no emergency occurs, and they are highly useful if emergency contingencies materialize at a fixed event as happened at and after the 2013 Boston Marathon. Skills honed at such events can also prepare responders and response organizations to perform more effectively even in “no notice” emergencies that may occur at other times.Furthermore, they recommend that emergency management agencies:
Identify and use every significant fixed event (such as parades, conventions, sporting events, and Fourth of July celebrations) as an opportunity to conduct joint planning and coordinated action involving all relevant agencies and disciplines. Engagement in these recurrent processes are a way to build mutual respect across agencies and disciplines by giving them the opportunity to see their colleagues’ professionalism and complementary skills and capabilities.The inherent link between emergency management and mass gatherings is reflected in the Victorian State Health Emergency Response Plan (SHERP):
SHERP provides a planning and management structure for public events and gatherings where there is potential for immediate mass casualties – and possibly increasing numbers of casualties over time. Involving health response agencies in pre-event planning may contribute to a safer, and therefore more successful, event. To this end it is recommended that events engage with health and medical providers that meet the requirements outlined in SHERP. (Victorian Government 2013)Mass gatherings are common in Australia. Events commonly coincide with peaks in natural hazard seasons and some of these events are held within high-risk geographic areas. In the absence of legislation and established systems there is no guarantee that emergency services and event organisers are aware of the others’ plans, operations and contact details. The impact of these events on local health, ambulance and emergency services is compounded further in rural and remote areas with limited pre-existing resources and inherently long transport times. This impact can often be safely and efficiently mitigated through planned health promotion, provision and protection strategies (Luke 2013, Luke & Dutch 2014, Dutch & Austin 2012). Herein lies a growing field of research, examining event characteristics, clinical presentations, public health implications and the development of predictive modelling and mitigation strategies (Arbon, Cusack & Verdonk 2013).
Large-scale Health deployments are inherently complex and should be managed with a whole-of-Health operational plan. Equipment, processes and skills can be built and refined through experience with mass gatherings and maintained in readiness for emergency response. Mass gatherings also provide an excellent and (usually) more controlled environment in which to gain operational and multi-agency command experience. Large international events such as the Olympic Games (2000), Commonwealth Games (2006, 2018), and World Youth Day (2008) provide additional cultural, language, security and public health challenges.
Health Department medical teams in Australia’s states and territories deployed for mass gatherings simultaneously exercise systems and provide hospital staff with pre-hospital clinical and multi-agency experience. Health involvement in large-scale events reduces the number of patients presenting to hospitals after the City 2 Surf run (NSW) and the Gold Coast Marathon and Schoolies Festival (QLD). Deploying additional, dedicated ambulance resources to events and emergency incidents reduces the use of local community ambulance resources while expediting patient stabilisation and transfer to hospital. Victorian Medical Assistance Teams were deployed during the 2009 bushfires and 2011 floods to support and augment rural health services. The New Zealand Territorial Services (military reserve) provide the medical team for Ironman New Zealand, giving clinicians valuable experience managing endurance illnesses also seen during military deployments. AusMAT medical teams use the gruelling Tour de Timor bike ride as a logistical and clinical training deployment (Luke 2013).
The way ahead
The introduction of a dedicated and elevated Health function within incident management structures would better acknowledge the importance and complexity of Health as a functional agency (Figure 2). Increased Health engagement in mainstream emergency management would drive the improvement of information-sharing systems, build stronger working relationships and improve insight into priorities, plans and systems. Mutual benefits would be expected to follow from increased collaboration in conference programming, shared training, and the development, maintenance and exercising of strategic plans.
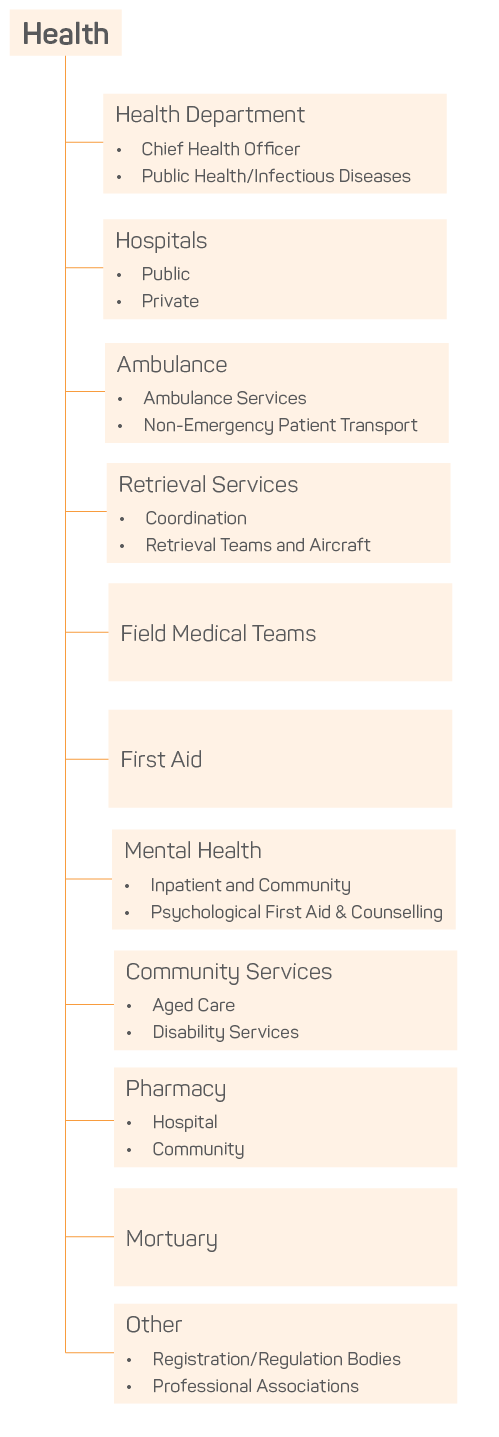
Figure 2: Proposed Health functional agency structure and component teams.
The adoption of established incident management principles and structure by Health emergency management would streamline inter-agency planning and operations. This would facilitate greater use of mass gatherings for exercising systems and gaining operational experience. The enforcement of these principles would also provide a solid foundation for greater regulation of event management. Elevating Health within incident management structures could provide stimulus to exercise, review and integrate government, health and hospital emergency management plans.
The question of Health functional agency leadership will inevitably arise and its solution is complex and the details beyond the scope of this discussion. Health command requires operational command experience and the ability to ‘speak emergency management’. But it is bigger than any one agency and requires specialist training, well-established professional networks and a working knowledge of hospital and health services. The fundamental principles of ‘All Hazards Incident Command’ and AIIMS Doctrine (Conway 2012) are equally applicable to everyday and disaster health management. It is important that the complexity of Health systems and command be included in mainstream command training.
For all their differences, mainstream and Health emergency management share many similarities, as evidenced by the parallel development of the ‘all hazards, all agencies’ and ‘whole-of-health’ response doctrines respectively. The elevation and integration of Health as an equal partner in incident management frameworks and resultant structures would have rapid and ongoing benefits in emergency and event planning and management.
As future reviews of our emergency management arrangements occur and in the spirit of Conway’s AIIMS Doctrine: have we got the fundamentals right? (Conway 2012), it is time to reflect on the benefits of making AIIMS and other incident management systems healthier.

The integration of Health as an equal partner in incident management frameworks has obvious benefits for event planning. Image: Stephen Luke.
References
AFAC 2013, AIIMS4: The Australasian Inter-Service Incident Management System: Australasian Fire and Emergency Service Authorities Council.
Arbon P, Cusack L & Verdonk N 2013, Mass Gathering Public Health and Emergency Medicine Literature Review: Levels of Evidence. Australasian Journal of Paramedicine, 10(1).
Australian Govternment 2011, Severe Burn Injury Annex to AUSTRAUMAPLAN. Canberra, Australia.
Bradt DA, Bartley B, Hibble BA & Varshney K 2015, Australasian disasters of national significance: An epidemiological analysis, 1900-2012. Emergency Medicine Australasia, vol. 27, no. 2, pp. 132-138.
Conway G 2012, AIIMS Doctrine: have we got the fundamentals right? Australian Journal of Emergency Management, vol. 27, no. 2, pp. 54-57.
Dean S 2015, Ravenshoe Café explosion: Tuesday 9 June 2015. Australian Journal of Emergency Management, vol. 30. no. 3, p. 35.
Dutch MJ & Austin KB 2012, Hospital in the Field: Prehospital Management of GHB Intoxication by Medical Assistance Teams. Prehospital and disaster medicine, 1-5. doi: 10.1017/S1049023X12000994.
Garlick D 2015, The Vulnerable People in Emergencies Policy: hiding vulnerable people in plain sight. Australian Journal of Emergency Management, vol. 30, no. 1, pp. 31-34.
Kohn EP 2010, Hot Time in the Old Town: The Great Heat Wave of 1896 and the Making of Theodore Roosevelt: Perseus Books Group.
Leonard HB “Dutch”, Cole CM, Howitt AM & Heymann PB 2014, Why was Boston Strong? Lessons from the Boston Marathon Bombing Program on Crisis Leadership. Cambridge, Massachusetts: John F. Kennedy School of Government, Harvard University.
Little M, Stone T, Stone R, Burns J, Reeves J, Cullen P, Humble I, Finn E, Aitkin, P, Elcock M, Gillard N 2012, The evacuation of Cairns hospital due to Severe Tropical Cyclone Yasi. Academic Emergency Medicine, 19(9), E1088-E1098.
Luke SRG 2013, Mass Gatherings: Health Promotion, Provision &Protection (pp. 1-133): Emergency Services Foundation.
Luke SRG & Dutch MJ 2014, Extreme Sporting Events and Transport Mitigating Strategies: An Australian Perspective. Annals of Emergency Medicine, vol. 64, no. 2, pp. 215-216.
National Critical Care and Trauma Response Centre (NCCTRC) 2015, National Critical Care and Trauma Response Centre. At: www.nationaltraumacentre.nt.gov.au.
PricewaterhouseCoopers (PWC) 2011, Protecting human health and safety during severe and extreme heat events. A national framework. PricewaterhouseCoopers Australia.
Queensland Government 2016, The Ravenshoe Review. Brisbane, Queensland Government. At: www.health.qld.gov.au/research-reports/reports/ravenshoe-review/documents/ravenshoe-review.pdf.
UNISDR 2005, Hyogo Framework for Action 2005-2015: Building the Resilience of Nations and Communities to Disasters. Geneva, Switzerland: United Nations. At: www.unisdr.org/2005/wcdr/intergover/official-doc/L-docs/Hyogo-framework-for-action-english.pdf.
UNISDR 2015, Sendai Framework for Disaster Risk Reduction 2015-2030. Geneva, Switzerland: United Nations. At: www.preventionweb.net/files/43291_sendaiframeworkfordrren.pdf.
Victorian Government 2013, State Health Emergency Response Plan (3rd Edition). Melbourne, Victoria. At: www.health.vic.gov.au/sherp/.
Victorian Government 2014, State Heat Plan. Melbourne, Victoria. At: www.emv.vic.gov.au/plans/state-heat-plan/.
About the author
Stephen Luke is a critical care doctor with 15 years operational event and emergency management experience. His Emergency Services Foundation scholarship project examined health command and deployment models in the UK, New Zealand and around Australia. He has been a St John Ambulance volunteer for over 20 years.


